Prior to the COVID-19 pandemic it may have been primarily researchers in labs and clinicians in intensive care units who were aware of a dangerous form of infection-triggered runaway inflammation known as a cytokine storm. But when cytokine storm reactions linked with COVID-19 started claiming lives by the thousands, scientists mobilized to try to find potential therapeutic answers.
A study led by immunobiology experts at Cincinnati Children’s, and described in Cell Reports “Effector memory T cells induce innate inflammation by triggering DNA damage and a non-canonical STING pathway in dendritic cells,” has now unveiled what the researchers suggest are important new details on how two elements of the body’s immune system clash with each other to prompt a chain of reactions that can release deadly floods of cell-killing, organ-damaging cytokines.
“These findings have implications for both autoimmunity as well as cancer,” said co-corresponding author Chandrashekhar Pasare, DVM, PhD, director of the division of immunobiology and co-director of the Center for Inflammation and Tolerance at Cincinnati Children’s. “We have discovered an independent cell signaling pathway that allows a type of immune cell called an effector memory T cell (TEM) to become a critical driver of innate cytokine storms.”
The chain reaction leading to a cytokine storm appears to start when the effector memory T cells interact with dendritic cells. These starburst shaped cells carry a large collection of receptors to detect various types of invaders. Once they encounter a harmful visitor, dendritic cells latch on and sound an alarm that instructs the rest of the immune system’s machinery to begin producing T cells that are custom designed to eliminate that type of invader.
When the immune system wins the battle, most of the custom T cells stand down. As well as triggering the differentiation of effector T cells that fight the primary infection, the immune system also generates long-lived effector memory T cells that can then respond quickly when they meet DCs carrying signals of reinfection. However, they also have the potential to induce inflammatory responses, the researchers noted.
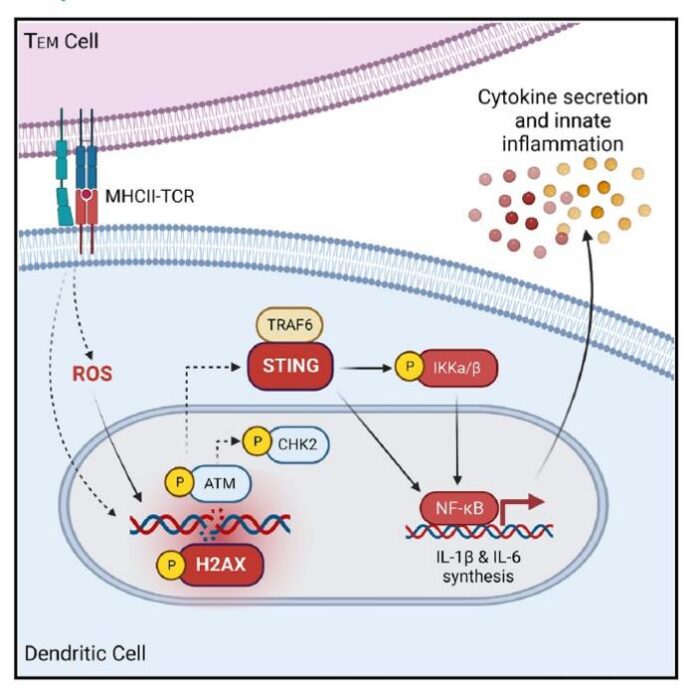
The scientists have now discovered that ongoing encounters with TEM cells, such as those occurring when people have autoimmunity or live in a state of chronic inflammation, actually cause DNA strands within dendritic cells to break. This, in turn, prompts a DNA repair pathway that rapidly generates large numbers of inflammatory cytokines, including IL-1b, IL-6 and IL-12.
This flood, or storm, of cytokines causes the tissue damage that occurs in autoinflammatory diseases including type 1 diabetes, multiple sclerosis, rheumatoid arthritis, and inflammatory bowel diseases such as Crohn’s disease. For some people with these conditions, ongoing inflammation also increases their risk of developing cancer.
Pasare and colleagues worked for the last 10 years to examine the genetic activity and cell-to-cell communications occurring behind this process. Together with their collaborators, the team found a surprising clue when examining the transcriptional profile of dendritic cells following their interaction with TEM cells. Specifically, they detected upregulation of expression of Tmem173, which encodes for stimulator of interferon genes (STING). The STING pathway has been described in previous research as being important to detect viral infections. But when TEM cells harm dendritic cells, the STING pathway does not follow the same route that it typically does when directly responding to viral infections. The results of their tests, they noted, “suggested an alternate, non-canonical role of STING during TEM cell-induced innate inflammation.”
In this situation, they found, STING teams up with the gene TRAF6 and the transcription factor NFkB to form an “axis” of activity that drives runaway production of innate inflammatory cytokines. The researchers further reasoned that if they could prevent STING and TRAF6 from working together, they could cut off the inflammation chain reaction at an early stage. In mice gene-edited to lack the STING pathway, that’s exactly what they found. When treated with a drug known to induce an intense T cell-mediated inflammatory response, these animals did not produce a flood of innate cytokines. The findings from a collective in vivo, as well as in vitro studies, provided what the authors suggested is “compelling evidence to establish STING as a major driver of T cell-induced inflammation in DCs, and these results have important implications for targeting STING for autoimmune and autoinflammatory diseases.”
The mouse study involved a whole-body elimination of STING. Attempting the same in humans would not be advisable because STING is used by a number of cell types outside the immune system in necessary ways, Pasare acknowledged. “STING is a widely expressed protein, and its diverse functional roles in multiple cell types pose a challenge for therapeutic targeting,” the team stated. Nevertheless, they suggested, “The discovery of TEM cell-induced innate inflammation through DNA damage and a non-canonical STING-NF-kB pathway presents this pathway as a potential target to alleviate T cell-driven inflammation in autoimmunity and cytokine storms … It would be especially beneficial to preserve the anti-viral activity of STING and specifically target its ability to complex with TRAF6 to prevent TEM cell-induced inflammation.”
With a pathway defined, the next steps will include further study to confirm whether medications that target key points along the pathway can disrupt the inflammation cycle before it becomes uncontrollable, Pasare suggested. “The discovery of TEM cell-induced innate inflammation through DNA damage and a non-canonical STING-NF-kB pathway presents this pathway as a potential target to alleviate T cell-driven inflammation in autoimmunity and cytokine storms,” the authors noted. “Our goal will be to develop a highly focused method or methods for blocking STING within targeted immune cells, without disrupting its other important functions. If we can achieve that, we may have a powerful new tool for controlling hyper-inflammation,” Pasare said.
Cincinnati Children’s co-authors on the reported study included first author Hannah Meibers, PhD, together with Kathrynne Warrick, Andrew VonHandorf, PhD, Charles Vallez, Kiana Kawarizadeh, Irene Saha, PhD, Omer Donmez, Viral Jain, MD, (now with the University of Alabama at Birmingham), Leah Kottyan, PhD, and Matthew Weirauch, PhD.