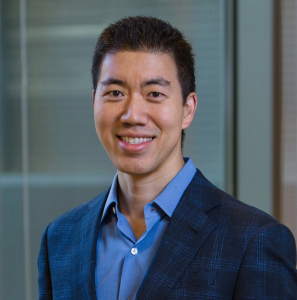
A new study published in Nature provides further validation for the therapeutic potential of base editing, a relatively new genome editing technology developed by David Liu, PhD, and colleagues at the Broad Institute, Harvard University, and the Howard Hughes Medical Institute.
In the new article, Liu’s group, in collaboration with NIH director Francis Collins, MD, PhD, have successfully treated the genetic mutation in a mouse model of progeria, a form of premature aging. GEN previously reported the highlights of this work in early 2020, after Liu presented his team’s progress at a scientific conference.
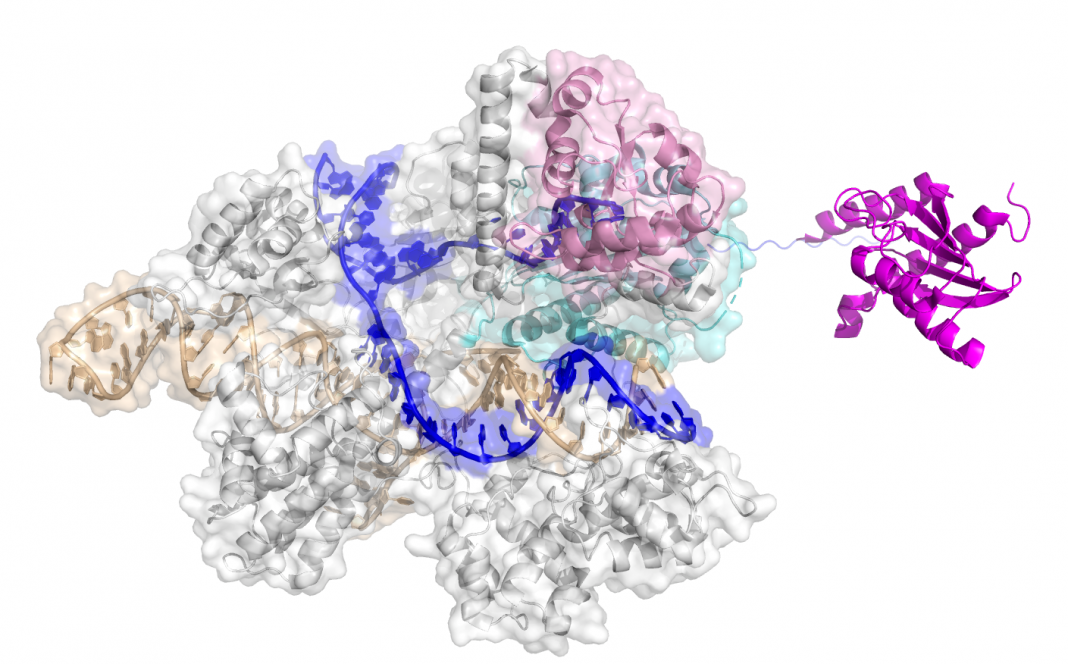
The new work seeks to treat a mouse model of Hutchinson-Gilford progeria syndrome (HGPS), a Mendelian disorder that results in premature aging. Most HGPS patients do not live beyond 15 years of age. Although a rare dominantly inherited disorder, most HGPS patients possess the same mutation—a C-to-T mutation in the nuclear lamin A gene. This sets up the disease as a candidate for treatment using adenine base editors (ABEs), developed by Nicole Gaudelli, PhD, and colleagues in Liu’s group a few years ago. Base editors are capable of engineering precise base substitutions to repair a genetic defect.
Grad student Luke Koblan, Michael Erdos, PhD, and their colleagues used an ABE to correct the pathogenic mutation in a mouse model of HGPS as well as cultured cells of HGPS patients. The authors used lentivirus vectors to deliver the ABE into patient fibroblasts, generating about 90% correction, reduced production of the aberrant progerin protein, and no detectable off-target effects.
In the mouse model, the researchers used an adeno-associated virus to deliver the ABE. Levels of mutation correction were 20–60% in various organs; the investigators also recorded lowering of progerin levels and restoration of normal vascular pathology. Strikingly, a single injection of ABE into mice two weeks after birth not only enhanced animal activity but also more than doubled the animals’ lifespan, from 215 days to 510 days.

“The toll of this devastating illness on affected children and their families cannot be overstated,” Collins said in a press release. “The fact that a single specific mutation causes the disease in nearly all affected children made us realize that we might have tools to fix the root cause.” He added that the crucial base editing technology was only developed thanks to long-term government investment in basic genomics research.
“It’s incredibly exciting to think that an idea you’ve been working on in the laboratory might actually have therapeutic benefit,” said Jonathan Brown, MD, a study co-author and assistant professor of medicine in the division of cardiovascular medicine at Vanderbilt University Medical Center. “Ultimately our goal will be to try to develop this for humans, but there are additional key questions that we need to first address in these model systems.”
The new results are encouraging in themselves, but the authors highlight further reasons for optimism. Since the genesis of the Nature report, Liu and coworkers have developed a suite of advanced ABE reagents with much greater activity. And progress is being made in other forms of drug therapy for progeria, which could complement the ABE approach, including the approval of a new drug in late 2020.
In an accompanying News & Views article, Wilbert Vermeij, PhD, and Jan Hoeijmakers, PhD, strike a positive note. “If base editing is to be used to treat human disease, the safety of such an intervention must be ensured. If it can be, and if this method successfully repairs the progeria-causing alteration in the crucial tissues, such an approach holds tremendous promise as a way of prolonging health, extending lifespan, and improving the quality of life of those who have this mutation.”