The sequencing of the human genome promised a revolution in medicine, but scientists soon realized that a genetic blueprint alone does not show the body in action. The lipidome may be filling out more details of human physiology that are not fully seen in the human genome. A new study from the lab of Michael Snyder, PhD, the Stanford W. Ascherman, MD, FACS professor in genetics, is among the first to deeply dive into the human lipidome and track how it changes under healthy and diseased conditions, particularly in the development of type 2 diabetes.
“Lipids are very understudied,” explained Snyder. “They are involved in pretty much everything, but because they’re so heterogeneous, and there are so many of them, we probably don’t know what most lipids really do.”
The findings are published in Nature Metabolism in an article titled, “Dynamic lipidome alterations associated with human health, disease, and aging.”
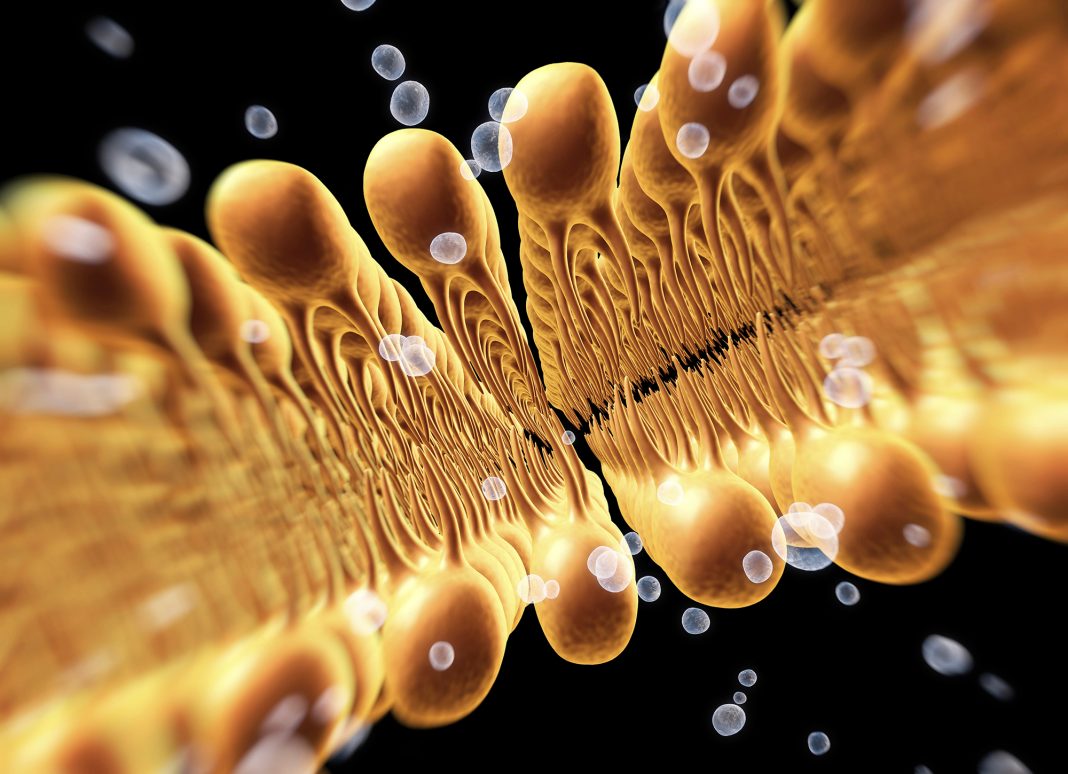
Lipids are a broad category of small, fatty or oily molecules, including triglycerides, cholesterol, hormones, and some vitamins. In our bodies, they make up cell membranes, act as cellular messengers, and store energy; they also play key roles in responding to infection and regulating our metabolism.
More than 100 participants, including many at risk for diabetes, were tracked for up to nine years, providing blood samples every three months when healthy and every few days during illness.
Using mass spectrometry techniques, the researchers cataloged some 800 lipids and their associations with insulin resistance, viral infection, aging, and more. The researchers discovered that although everyone’s lipidome has a distinctive signature that remains stable over time, certain types of lipids changed predictably with a person’s health.
“Every molecule that is associated with a disease has a chance of telling us more about the mechanism and may be serving as a target for affecting the disease progression,” said Daniel Hornburg, PhD, a former postdoctoral scholar in Snyder’s lab and co-lead author of the study.
The researchers also identified more than 200 lipids that fluctuate over the course of a respiratory viral infection. Rising and falling levels of these lipids matched the body’s higher energy metabolism and inflammation in early infection, and may indicate the trajectory of the disease. Those with insulin resistance showed some anomalies in these responses to infection as well as a weaker response to vaccinations.
Next, Snyder’s lab hopes to follow leads from this broad survey to look at correlations between specific lipids and lifestyle changes.