Infectious diseases, believed to be a thing of the past only a few decades ago owing to the discovery of antibiotics, have resurfaced as an area of active research with the rampant spread of antimicrobial resistance and evolving viruses. Caused by pathogens ranging in size from viruses to worms that infect larger host organisms, the hallmark of infectious diseases is transmissibility. The outcome of an infection depends on the cellular and molecular interplay between pathogen and host and can result in either asymptomatic commensal colonization of the host by the pathogen, or symptomatic colonization leading to prolonged disease or death of the host.
New research methods are being continuously developed and refined to better understand complex molecular events in infection cycles, determinants of pathogenesis, and host immune responses, with the aim of exploiting vulnerabilities in pathogens and identifying druggable targets in hosts to treat clinical manifestations of infectious diseases.
“Spatial transcriptomics, high-content analysis, organoids and organ-on-chip platforms, functional genomic screening, and AlphaLISA protein-protein interaction assays are the top methods that will advance our understanding of infectious diseases research and drug discovery,” says Karin Boettcher, PhD, strategy leader of life science research at PerkinElmer, who did her doctoral and postdoctoral work in microbiology and parasitology at the University of Goettingen, Germany.
Spatial insights into infection
Recent innovations in spatial transcriptomics have provided new insights into infectious disease biology by enabling the analysis of gene expression at the single-cell level while maintaining morphological context of the tissue. This not only allows exhaustive cataloging of cells present at sites of infection in the host, but also analyses of signal transduction mechanisms that permit or promote pathogen survival in microenvironmental niches in the host.
“Elucidating host-pathogen interaction at a cellular and molecular level to facilitate patient stratification and clinical decision-making requires next-generation methodologies, especially given the rapid introduction of new therapies,” says Boettcher. “Automated confocal imaging combined with quantitative image analysis is very important in making the analysis of large tissue sections feasible. However, spatial transcriptomics requires human or mouse tissue samples which might not always be available.”
Relevant models
A prerequisite to studying pathogens, including viruses such as SARS-CoV-2 and their variants, is the ability to culture such pathogens in vitro. A conventional approach to developing cell culture models for new pathogens has been to genetically engineer cell lines to express the host membrane receptor that the virus uses to enter the host. “However, these cell lines are not physiologically relevant and not informative about virus or pathogen biology in vivo,” Boettcher cautions.
For example, the human lung-derived cell line MRC5, which is highly susceptible to infection by human coronaviruses 229E and OC43, is resistant to SARS-CoV-2. Therefore, scientists have stably transfected MRC51 cells with a lentiviral vector encoding angiotensin-converting enzyme 2 (ACE2) to induce viral infection and replication in these cells and used these mutagenized cells as models for the development of antiviral and vaccines.
“Advanced cell culture models such as iPSC (induced pluripotent stem cell) derived organoids or organ-on-chip platforms encompassing several cell types of the target organ as well as immune cells are critical for disease modeling and identification of new treatment options,” says Boettcher.
The use of physiologically relevant cell culture models has been limited in infectious disease research until now, but COVID-19 has initiated new investigations in this direction. SARS-CoV-2 infections have been explored in airway-on-chip models, as well as human bronchial, kidney, intestinal, liver ductal, and brain organoids.
High-content analysis
Physiologically relevant, complex cell culture models are just the first step. To interrogate these models, one needs effective imaging and analytical tools such as high-content screening and analysis (HCS/HCA). This combines high-speed automated imaging at single-cell resolution with parallel pixel analysis to extract actionable data from infected cellular or organoid models.
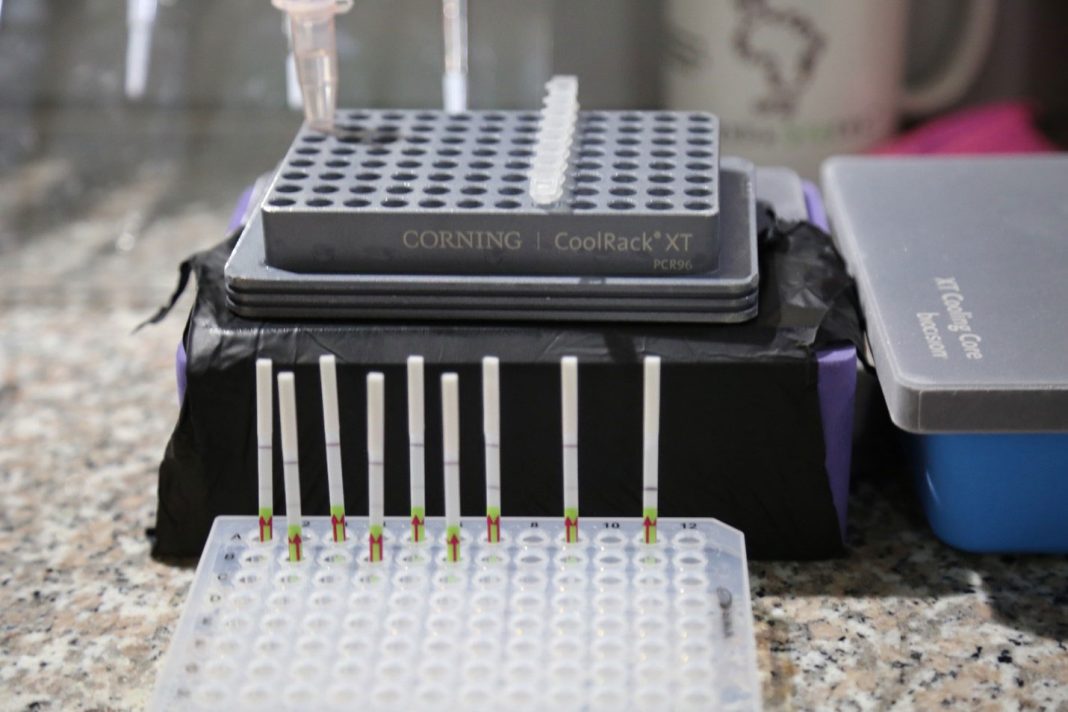
“While keeping the cell models intact, HCS allows multiplexed readouts, such as the extent of infection, target cell types, morphologies of host cells, and much more,” says Boettcher. “Infectious disease researchers having used qPCR in the past to quantify infections, love the fact that all this information can be collected in a single well in one experiment.”
HCA has enabled studies on HIV-associated neurocognitive disorders (HAND) to decipher the effects on various therapeutic agents such as nucleoside/nucleotide reverse transcriptase inhibitors on the viability, structure, and function of glutamatergic neurons and primary human neural precursor cells.2
Host-pathogen interactions
Some pathogens, such as viruses, need the cooperation of factors in the host cell to establish infection. Targeting allied factors in the host constitutes a viable strategy to inhibit such pathogens. A key advantage to targeting the host rather than pathogen proteins to contain infection, is that compared to virus or parasite proteins, host proteins are less prone to mutations. Host-directed therapeutics, therefore, are less prone to drug resistance. Moreover, targeting host factors that act as gatekeepers could potentially inhibit entire families of pathogens rather than a single culprit.
“Elucidating essential host cell proteins and protein interactions between pathogen and host cell proteins is key to finding innovative drug targets,” says Boettcher.
CRISPR or siRNA-based functional genomic screens on whole genomes have been used to understand host-pathogen interactions for several key pathogens, including Zika virus, Dengue virus, and SARS-CoV-2.3 These approaches continue to be key in infectious disease research and drug discovery.
Once a molecular interaction has been detected between a viral component and a virus interacting protein (VIP)—a host cell protein that physically binds a viral protein, RNA, and/or DNA—it needs to be validated using multiple parallel assays that can be scaled up for high-throughput drug screening.
“This can be achieved with AlphaLISA protein-protein interaction (PPI) assays that enable PPI inhibition screening at scale,” says Boettcher. “AlphaLISA assays have been used to confirm SARS-CoV-2 and Zika VIPs.”
Therapeutic strategies
Infectious diseases are a global public health concern, and the convenience of air travel creates ample opportunity for the rapid spread of infections across physical and political borders. Yet certain infectious disease shows distinct regional preferences. For example, malaria is caused by the protozoan Plasmodium falciparum which is endemic to tropical countries.
Although therapeutic strategies against infectious diseases target either the pathogen or the host, these approaches are modulated by management of clinical manifestations and complexities of host-pathogen interaction, particularly the effect of sup-optimal host immune responses on the evolution of pathogen species that “learn” to express surface proteins to evade future host immune attacks.
“Traditionally, antibiotics are used to treat bacterial infections, antimicrobials against fungi or parasites, and antiviral agents to combat viruses. Therapeutic compounds or biologics either treat or diminish the symptoms of specific infectious diseases. Preventive measures such as vaccines have been successful in either preventing infection or minimizing the symptoms of the disease,” says Anis Khimani, PhD, senior strategy leader of life sciences at PerkinElmer, and who has conducted research in virology, pathogenesis, and vaccines at Harvard Medical School, Dana-Farber Cancer Institute, and at the Boots Pharmaceutical Company in U.K., and India.
The past decade has witnessed the rapid development of immunotherapies, including monoclonal antibodies, T-cell therapies, checkpoint inhibitors, and RNA-based therapies. Checkpoint inhibition, previously solely used in cancer treatment, is now a viable treatment option for infectious diseases such hepatitis B virus (HBV) infections.4
Innovations to combat drug resistance
The emergence of resistance of pathogens against existing therapeutics is a key impetus for continued innovation in drug discovery and repurposing approved or pipeline candidates for other indications.
“Resistance to drugs is noted across a number of infectious disease pathogens such as tuberculosis, hospital-acquired infections, malaria, and HIV,” says Khimani. “For example, emerging strains of HIV have been identified that are resistant to the multiple drug anti-retroviral therapy (ART).” Strains of HIV resistant to ART, therefore, require new drugs.
Reverse vaccinology, driven by artificial intelligence and structure-guided immunogen design, has been recently used to design vaccines against SARS-CoV-2 and other pathogens. It is a bioinformatic approach that screens all genes in a pathogen to identify those that confer antigenicity—the capacity of a chemical structure, usually on the surface of a pathogen to trigger an immune response in the host, and other desirable features for vaccine targets. Reverse vaccinology helps identify new vaccine candidates that are then synthesized and screened in vivo.
“Leveraging AI can also expedite clinical research and trials streamlining the process and subsequent monitoring,” says Khimani.
Vaccines, monoclonal antibodies, and checkpoint inhibitors continue to be explored against viral, bacterial, and parasite infections. In addition to the use of attenuated whole pathogens, vaccines now include mRNAs and plasmid-DNAs that have been used against a range of parasitic infections such as malaria, leishmaniasis, and toxoplasmosis.
“Nucleic acid vaccines can stimulate innate and adaptive immune responses and can overcome limitations encountered by peptide vaccines,” says Khimani.
Monoclonal antibodies, on the other hand, are designed to directly neutralize the pathogen, or to ease inflammation that follows infection. Khimani says, “For example, the anti-IL6 mAb, Tocilizumab, has shown to demonstrate efficacy in cases with cytokine storm following infection with SARS-CoV-2. Also, monoclonal antibodies against P. aeruginosa and S. aureus are in development, with potential for a broad-spectrum effectivity across isolates.”
Although still early in their development, antibody-antibiotic conjugates (AACs) are an emerging class of biotherapeutics for infectious diseases that ensure targeted delivery of antibiotics against bacterial infections. “Strategies combining novel immunotherapy targeting with conventional therapy show promising outcomes with more resilient pathogens, as well as potentially a broader coverage across variants within the same family of infectious agents,” adds Khimani.
The growing specter of drug resistance compounded by the emergence of new pathogens will require cross-disciplinary technical strategies not only in basic infectious diseases research but in developing effective therapeutics that give our species a winning chance in future host-pathogen feuds.
References
- Uemura K, Sasaki M, Sanaki T, et al. MRC5 cells engineered to express ACE2 serve as a model system for the discovery of antivirals targeting SARS-CoV-2. Sci Rep. 2021 Mar 8;11(1):5376.
- Smith AS, Ankam S, Farhy C, et al. High-content analysis and Kinetic Image Cytometry identify toxicity and epigenetic effects of HIV antiretrovirals on human iPSC-neurons and primary neural precursor cells. J Pharmacol Toxicol Methods. 2022 Mar-Apr;114:107157.
- Gootenberg JS, Abudayyeh OO, Lee JW, et al. Nucleic acid detection with CRISPR-Cas13a/C2c2. Science. 2017 Apr 28;356(6336):438-442.
- Chen Y, Tian Z. HBV-Induced Immune Imbalance in the Development of HCC. Front Immunol. 2019 Aug 27;10:2048.
- Stagg NJ, Katavolos P, Achilles Poon K, et al. Nonclinical toxicology development of a novel antibody antibiotic conjugate for treating invasive Staphylococcus Aureus infections. Toxicol Appl Pharmacol. 2022 Jan 15;435:115811.