Antiviral therapies are notoriously difficult to develop, as viruses can quickly mutate to become resistant to drugs, or hide within cells. Researchers at NYU have now developed a new approach to antiviral treatment that ignores the fast-mutating proteins on the surface of viruses and instead targets lipids in the membranes of enveloped viruses, which disrupts their protective layers. In a newly published study the researchers showed how these novel peptoid molecules, inspired by the immune system, could inactivate several viruses, including Zika and chikungunya. The team suggests their approach may not only lead to drugs that can be used against many viruses, but could also help overcome antiviral resistance.
“We found an Achilles heel of many viruses: their bubble-like membranes,” said Kent Kirshenbaum, PhD, professor of chemistry at NYU. “Exploiting this vulnerability and disrupting the membrane is a promising mechanism of action for developing new antivirals.” Kirshenbaum is senior author of the team’s published paper in ACS Infectious Diseases, which is titled “Peptidomimetic Oligomers Targeting Membrane Phosphatidylserine Exhibit Broad Antiviral Activity.”
In their paper the authors concluded, “We provide the first evidence for the engagement of distinct viral envelope lipid constituents, establishing an avenue for specificity that may enable the development of a new family of therapeutics capable of averting the rapid development of resistance.”
Viruses have different proteins on their surfaces that are commonly targets of therapeutics such as monoclonal antibodies and vaccines. But targeting these proteins has limitations, as viruses can quickly evolve, changing the properties of the proteins and making treatment less effective. These limitations were evident when new SARS-CoV-2 variants emerged that evaded both the drugs and the vaccines developed against the original virus. “The emergence of COVID variants is indicative of the general challenges in establishing robust treatment regimens for viruses of pandemic potential,” the authors pointed out. One avenue for addressing these challenges is to identify therapeutic targets that are conserved and specific to the virus and are non-toxic to host cells.”
Kirshenbaum added, “There is an urgent need for antiviral agents that act in new ways to inactivate viruses. Ideally, new antivirals won’t be specific to one virus or protein, so they will be ready to treat new viruses that emerge without delay and will be able to overcome the development of resistance … We need to develop this next generation of drugs now and have them on the shelves in order to be ready for the next pandemic threat—and there will be another one, for sure.”
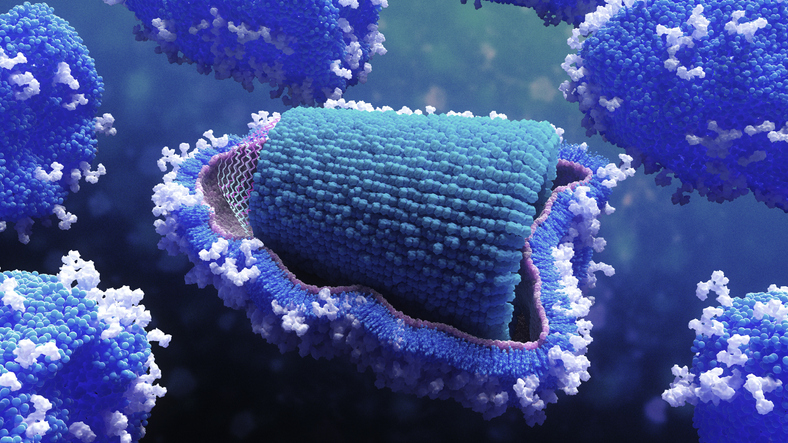
The innate immune system combats pathogens by producing antimicrobial peptides (AMPs), the body’s first line of defense against bacteria, fungi, and viruses. Most viruses that cause disease are encapsulated in membranes made of lipids, and antimicrobial peptides work by disrupting or even bursting these membranes.
While antimicrobial peptides can be synthesized in the lab, they are rarely used to treat infectious diseases in humans because they break down easily, can be toxic to healthy cells, and are expensive to produce. Instead, scientists have developed synthetic peptoids (“N-alkylated glycine oligomers”), which are sequence-specific peptidomimetic compounds that have similar chemical backbones to peptides but are better able to break through virus membranes and are less likely to degrade. They are also more economical to produce. “Relative to peptides, peptoids have greater membrane permeability and are not prone to proteolytic degradation,” the team noted. “We began to think about how to mimic natural peptides and create molecules with many of the same structural and functional features as peptides, but are composed of something that our bodies won’t be able to rapidly degrade,” added Kirshenbaum.
Study co-author Annelise Barron’s team at Stanford had previously shown that certain peptoids could pierce and destroy the SARS-CoV-2 and herpes viruses. For their newly reported study the group wanted to see if peptoids could inactivate three other enveloped viruses enclosed within membranes—Zika, Rift Valley fever and chikungunya virus—as well as one that lacks a membrane envelope, coxsackie B3.
“We were particularly interested in studying these viruses as they have no available treatment options,” said Patrick Tate, a chemistry PhD student at NYU and the study’s first author. The membranes surrounding viruses are made of different molecules than the virus itself, as lipids are acquired from the host to form membranes. One such lipid, phosphatidylserine, is present in the membrane on the outside of viruses, but is sequestered towards the interior of human cells under normal conditions.
“Because phosphatidylserine is found on the exterior of viruses, it can be a specific target for peptoids to recognize viruses, but not recognize—and therefore spare—our own cells,” said Tate. “Moreover, because viruses acquire lipids from the host rather than encoding from their own genomes, they have better potential to avoid antiviral resistance.”
The researchers tested seven peptoids against the four viruses. The peptoids used included three of the linear peptoids previously studied by Barron’s team, as well as four new circularized versions with increased antiviral activity. The researchers created model virus membranes using common lipids, and found that the peptoids could inactivate all three enveloped viruses—Zika, Rift Valley fever, and chikungunya—by disrupting the virus membrane, but did not disrupt coxsackievirus B3, the only virus without a membrane.
Moreover, membranes containing higher levels of phosphatidylserine (PS) were more susceptible to the peptoids. In contrast, a membrane formed exclusively with a different lipid, phosphatidylcholine was not disrupted by the peptoids, suggesting that phosphatidylserine is crucial in order for peptoids to reduce viral activity. “We found that liposomes containing phosphatidylserine (PS) were markedly sensitive to peptoid treatment; in contrast, liposomes formed exclusively with phosphatidylcholine (PC) showed no sensitivity,” the team stated. “In addition, chikungunya virus containing elevated envelope PS was more susceptible to peptoid-mediated inactivation.”
Next, the team incubated the peptoids with whole, infectious virus particles. Again, each worked to a different extent on the three enveloped viruses: some of the peptoids disrupted all three, some only one. However, none of the peptoids could inactivate the non-enveloped coxsackie B3 virus, showing that the mechanism of action hinges on the presence of the viral envelope. “Most notably, all three enveloped viruses were susceptible to peptoid-mediated inactivation, whereas CVB3, the only non-enveloped virus, remained impervious to peptoid treatment,” they stated.
The team says that understanding this mechanism of peptoid activity could inform the design of future peptoid-based antiviral treatments, and could be used to create drugs already armed against the next emerging viral threat. “We’re now starting to understand how peptoids actually exert their antiviral effect—specifically, through the recognition of phosphatidylserine,” said Tate. “Our results indicate that certain amphiphilic peptoid oligomers can mimic AMPs and exert antiviral activity through a membrane disruptive mechanism,” the team further stated. “Furthermore, the presence of PS appears to be critical for peptoid-mediated activity.”
The researchers are continuing preclinical studies to evaluate the potential of these molecules in fighting viruses and to understand if they can overcome the development of resistance. The peptoid-focused approach may hold promise for treating a wide range of viruses with membranes that can be difficult to treat, including Ebola, SARS-CoV-2, and herpes. “As viruses obtain lipids from their host during replication and do not genetically encode their own lipid constituents, targeting the membrane bilayer of enveloped viruses offers a pathway toward effective therapeutics, which may prevent the generation of resistant variants,” the authors concluded. “Additionally, these compounds act directly on virus particles to disrupt their membranes, establishing potential countermeasures against newly emerging viral threats.”