A study in mice and in rabbits suggests that an experimental drug called saracatinib, which has already been tested as a potential treatment for cancer, lung, and Alzheimer’s disease, may slow the progression of atherosclerosis that leads to heart disease. To identify the drug as a potential candidate for atherosclerotic cardiovascular disease (ASCVD) investigators led by a team at NYU Grossman School of Medicine developed a strategy that combines systems immunology-driven-drug repurposing, with a functional screen using human samples.
Their initial experiments found that plasma from patients with atherosclerotic disease triggers an usually high inflammatory signal in blood immune cells, then showed that the drug saracatinib reduced this inflammation signaling by more than 90% in human blood samples and diseased tissue samples. The combined results from their in vitro, and subsequent in vivo preclinical testing indicated that saracatinib reduced atherosclerosis progression and inflammation, and reprogrammed reparative macrophages.
“Our findings provide new insight into the inflammatory mechanisms in atherosclerosis and suggest for the first time that saracatinib may offer an effective therapy in cases where standard therapy, in the form of statins, fails to help,” said Letizia Amadori, PhD, a senior research scientist at NYU Langone Health.
Amadori is co-lead author of the team’s published paper in Nature Cardiovascular Research, which is titled “Systems immunology-based drug repurposing framework to target inflammation in atherosclerosis.” In their paper the team noted, “In conclusion, our systems immunology-driven drug repurposing framework led to the identification of a use for an existing drug to aid the development of targeted immunotherapies for ASCVD … In conjunction with a rigorous preclinical validation platform in animal models, this system can aid the clinical translation of existing drugs with new cardiovascular indications tailored to individual patients.”
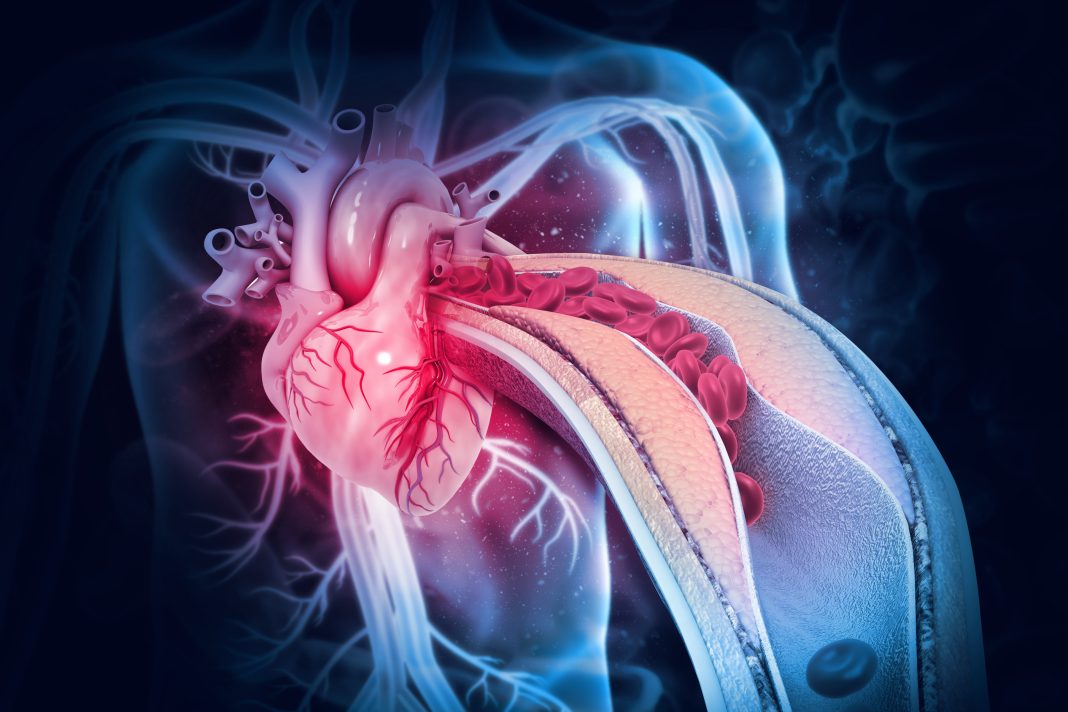
Atherosclerosis occurs when fatty deposits build up in blood vessels and hardens into plaques, which cause misplaced immune reactions (inflammation), and can block blood flow to cause heart attack or stroke. ASCVD is the leading cause of death worldwide, but progress in the development of new cardiovascular drugs has lagged behind that for other complex disease conditions, such as cancer, the authors noted. “Indeed, since the discovery of lipid-lowering statins and the recent PCSK9 inhibitors, drug innovation in the field has been stagnant.”
The current standard of care for ASCVD is to lower lipid levels and control other cardiovascular risk factors, such as diabetes, and hypertension. Physicians prescribe statins to reduce harmful fats in the blood, but studies show that even with reduced plaque deposits, inflammation persists in many patients, who remain at high risk for heart attack. The causes of this chronic immune response in patients are not fully understood, and anti-inflammatory treatments are sometimes ineffective in patient studies. Current treatments do not directly address the underlying inflammatory mechanisms of the disease.
For their newly reported study, the researchers explored the mechanisms behind atherosclerosis. They analyzed blood samples from 34 men and women with ASCVD—all of whom were on statins—and compared them with samples from 24 healthy donors.
Their initial analyses indicated that plasma from patients with atherslcerotic disease induced a strong and specific innate immune cell signaling responses in circulating inflammatory cells. They next exposed peripheral blood mononuclear cells (PBMCs) from healthy donors to plasma from individuals with ASCV, and observed a similar inflammatory response. The team then sequenced healthy peripheral blood mononuclear cells (PBMCs) stimulated using either atherosclerotic or healthy donor plasma. “To investigate the transcriptional changes associated with the phosphosignaling induced by atherosclerotic plasma, we performed RNA sequencing (RNA-seq) profiling of the same healthy PBMCs stimulated with the same atherosclerotic or healthy donor plasma. They identified 4,823 differentially expressed genes, including 277 already known to play a role in inflammation and produce cytokines and other proteins that promote a chronic immune response.
The investigators reasoned that if a drug could stop all these molecules from being made, could calm the response. However, rather than trying to create a suitable drug from scratch, the researchers instead turned to a list of pharmaceuticals already approved or being tested for other uses. Specifically, they searched a series of NIH datasets called the Library of Integrated Network-Based Cellular Signatures, which contains hundreds of thousands of test results mapping the effects of various molecules, signaling proteins, and genetic changes on human cells.
Saracatinib was identified as a top hit for its predicted ability to reverse the expression of target genes. The investigators then tested the drug—alongside other potential candidates identified—in human cells. Positive results from these tests prompted the team to continue to test saracatinib in diseased tissue. The combined results revealed that saracatinib blocks gene activity responsible for producing inflammatory proteins such as interleukin-1 beta and interluekin-6 that maintain ASCVD’s immune reactivity. Notably, the authors commented, an earlier trial had demonstrated that inhibitor of interleukin-1 beta effectively prevents heart attack.
At the same time, saracatinib boosted genes known to make proteins that help clean up plaque deposits by transporting fat away from the arteries. Commenting on the data from tests diseased tissues, the team stated, “.. these results suggest that saracatinib not only exerts anti-inflammatory and antiatherosclerotic effects on circulating immune cells but also directly on human atherosclerotic tissue.”
Following the positive in vitro data, the investigators evaluated saracatinib in animal models to see if it could stop, slow, or reverse inflammation prompted by ASCVD. “Based on these promising results, and due to its oral availability and safety profile in clinical trials, we selected the phase IIa-ready compound saracatinib for further investigation,” they stated. “Our in vivo studies were designed to test the hypothesis that saracatinib had an effect similar to that of atorvastatin in halting atherosclerosis inflammation progression versus placebo.”
Experiments in rabbits revealed that saracatinib reduced plaque-based inflammation by about 97%, compared with untreated animals. The same therapy mice prompted up to an 80% reduction in cells linked to inflammation in plaques and shrunk plaque deposits between 48% and 70%, depending on the dose of the medication. “In mice, saracatinib effectively reduced plaque burden and plaque inflammation, an effect that was superior to that of atorvastatin …” the authors noted. “In a rabbit model of atherosclerosis that generates complex human-like atherosclerotic plaques, aracatinib also had an anti-inflammatory effect on atherosclerotic lesions …”
Study senior author Chiara Giannarelli, MD, PhD, commented, “Our reverse-engineering method of finding new uses for old drugs can in theory be harnessed to uncover therapies for practically any disease that involves inflammation,” said. “Since these chemicals have already been tested for safety, this technique offers a swift and cost-effective approach to pharmaceutical development.” Giannarelli, an associate professor in the Departments of Medicine and Pathology at NYU Langone, says the study team next plans to use their same protocol to explore potential treatments for other inflammatory conditions linked to ASCVD, such as rheumatic arthritis or type 2 diabetes.
That said, Giannarelli cautions that while saracatinib appears promising, it must still be clinically tested to ensure that the treatment actually works in patients. The authors further noted, “By acting through different pathways, saracatinib has the potential to be used as an anti-inflammatory treatment for patients who are already treated with lipid-lowering drugs. This hypothesis will need to be tested in future Phase II clinical studies.”