Findings from the Garvan Institute of Medical Research and Pharmaxis, an Australian pharmaceutical research company, indicate that a new treatment for bone marrow cancer myelofibrosis currently in clinical trials may also work for pancreatic ductal adenocarcinoma (PDAC), one of the most aggressive forms of this type of cancer.
PXS-5505, a new oncology drug from Pharmaxis, is currently in Phase II clinical trial testing for bone marrow cancer cases. However, research involving mouse models of pancreatic cancer showed that when PXS-5505 was combined with chemotherapy, it increased survival time by more than 35% compared to treating with chemotherapy alone. The drug also reduced cancer metastases to organs like the liver by 45% in the test subjects.
Details of this preclinical study are available in a paper published in Nature Cancer.
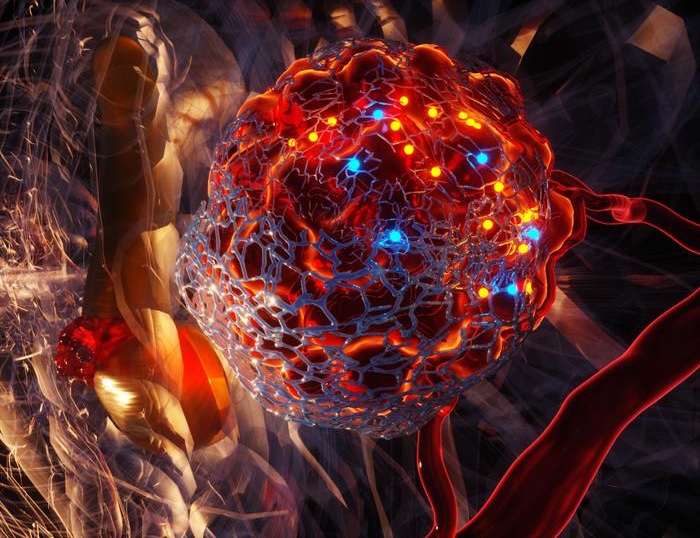
Pancreatic cancer often goes undiagnosed until it is quite advanced and chemotherapy is often the only viable treatment option. Unfortunately, many pancreatic cancers become resistant to treatment soon after in part due to a fibrotic mesh that forms within and around pancreatic tumors. This same scar-like tissue, which is also found in other solid cancers, limits the penetration of chemotherapies.
“Activation of tumor-associated stromal cells and increased deposition of the extracellular matrix in the tumor microenvironment is frequently associated with the aggressive nature of PDAC,” the researchers wrote in Nature Cancer. “Furthermore, there is growing recognition that many cancer therapies lead to exacerbation of fibrotic responses within tumors, further compounding these effects.”
Some current drug discovery studies are trying to target the mechanisms responsible for forming fibrotic tissue. One such target is a family of enzymes called lysyl oxidases which are involved in making the fibrillar collagens that form the fibrotic tissue. Prior studies have used small molecules that target single members of the family. However, these individualized therapies have met with limited success in trials.
PXS-5505 is different because it inhibits all members of the lysyl oxidase family that are involved in forming the fibrotic tissue. Pharmaxis has already completed long-term toxicity studies and Phase Ia and Ib clinical trials involving the drug with promising results. In July, the company released interim data from its Phase II clinical trials of PXS-5505 in patients with bone marrow cancer myelofibrosis.
According to the company’s data, the drug is well tolerated with no serious treatment-related adverse events. Patients also showed improved fibrosis scores and stable or improved hematological parameters after being on the drug for 24 weeks.
“PXS-5505 returns the tumor microenvironment to a more normal state by reducing fibrosis and decreasing tumor stiffness,” Jessica Chitty, PhD, senior research officer at Garvan and first author of the Nature Cancer study explained in a statement. “This allows chemotherapy drugs to penetrate the tumors more easily, work more effectively, and destroy more cancer cells.”
In the case of pancreatic cancer, results reported in the paper show that PXS-5505 successfully blocked lysyl oxidase family-mediated collagen crosslinking and reduced cancer cell invasion in both the mouse and human tumor models. The team also tested the effects of combining PXS-5505 with gemcitabine, a clinically approved chemotherapy. They observed a “statistically significant increase in median survival.” There was also a “significant reduction” in the fibrillar collagen content of the mouse tumors. The results were similar for the human patient-derived xenograft PDAC models. Importantly, PXS-5505 does not appear to interact with other human amine oxidases and seems to be well tolerated for about six months.
“The preclinical validation of this first-in-class anti-fibrotic drug marks a major milestone in our quest to overcome the significant challenges in treating pancreatic cancer and bring hope to patients and their families,” Thomas Cox, PhD, head of Garvan’s Matrix & Metastasis Lab, noted. Currently, less than 10% of pancreatic cancer patients have a five-year survival rate.
These results provide “exciting new evidence that PXS-5505 may also have a role as a therapy to improve the effect of current chemotherapy drugs in solid tumors like pancreatic cancer and [in] extending the life of patients,” he added.