Researchers at Purdue University have developed a new type of cancer therapy that uses a modified microRNA, miR-34a, to block cancer cell division. In preclinical tests in mice, treatment using the fully modified, tumor-targeting miR-34a halted tumor growth for the 21-day evaluation period, and resulted in complete cures in some animals. In contrast, untreated tumors tripled in size over the same time period. The miRNA construct was also invisible to the immune system, which would ordinarily attack double-stranded RNA introduced into the body.
Research lead Andrea Kasinski, PhD, the William and Patty Miller associate professor of biological sciences at Purdue University, told GEN clinical trials could feasibly start within two years, if the required, extensive efficacy, toxicity, and pharmacologic studies can be completed successfully. The initial clinical focus will be on triple-negative breast cancer (TBNC) and on non-small cell lung cancer (NSCLC).
Kasinski and colleagues reported on the findings from their murine studies in Oncogene, in a paper titled, “A first-in-class fully modified version of miR-34a with outstanding stability, activity, and anti-tumor efficacy,” in which they concluded, “These results have the ability to revitalize miR-34a as an anticancer agent, providing a strong rationale for clinical testing.” Kasinski further suggested, “Without question, the RNA therapeutics sector is expanding exponentially. The work we published is anticipated to revolutionize this area.”
MicroRNAs are short, noncoding RNAs that have the unique ability to downregulate multiple genes at the same time, and so miRNA-based therapeutics could represent promising potential tools for treating various diseases. And in the case of tumor suppressor miRNAs, one of the most clinically relevant is miRNA-34a, which regulates several oncogenic pathways that control cell proliferation, migration and invasion, resistance to apoptosis, and immune evasion, the investigators noted.
miRNA-34a effectively acts “like the brakes on a car,” stopping cell division, Kasinski said. But while microRNA-34a is abundant in healthy cells, its presence is dramatically reduced in many cancer cells. And as the investigators further noted, “Without question, a striking number of patients with cancer would benefit from miR-34a replacement.” However achieving this would depend on overcoming poor miR-34a stability, nonspecific delivery, and delivery-associated toxicity.
And it’s the challenges of specific delivery in the absence of toxicity, and poor stability of the RNAs that lead to the requirement for high, frequent dosing, that have been the main hurdles in developing a therapeutic miRNA-34a-based candidate, Kasinski further noted. “The first clinical trial using a microRNA (initiated in 2013) resulted in severe immune-related toxic events attributed to the delivery vehicle, high dosing needed to see an effect, and/or the unmodified microRNA that could elicit an immune response.”
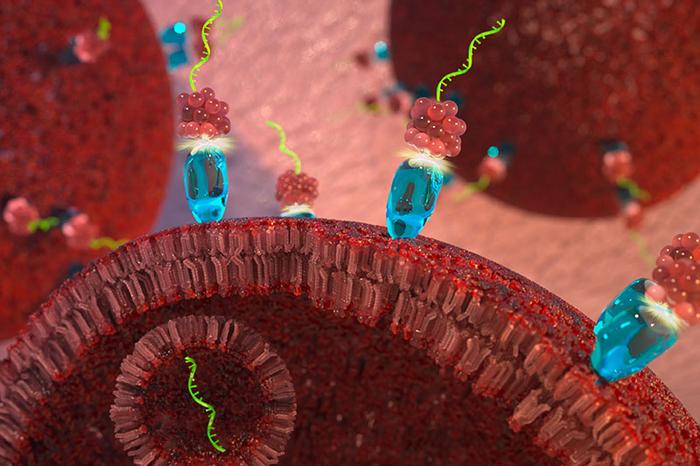
The research team spent a decade years working to overcome these key challenges in crafting an effective therapy, Kaskinski added. To ensure the modified microRNA-34a is delivered to cancer cells, the team attached the double RNA strand to a molecule of the vitamin folate. The surfaces of all cells in our body have receptors that bind to folate and draw the vitamin into the cell, but the cells in many cancers—breast, lung, ovarian, and cervical—have far more folate receptors on their cell surface than do healthy cells. “… we used a folate-miRNA delivery strategy, which allows for specific delivery of the miRNA to folate receptor (FR)-overexpressing tumors without the need for packaging the miRNA within a vehicle,” the scientists explained in their paper. This approach eliminates the “nonspecific, often toxic, and bulky delivery vehicle,” Kasinski further explained to GEN. “We were the first group to use a ligand-mediated delivery approach for delivering a microRNA.”
To improve the durability of therapy, the team stabilized microRNA-34a by adding several small clusters of atoms along the length of the strand. The team modeled its modifications on an FDA-approved chemical structure that is used with similar short-interfering RNAs. Experiments in mouse models showed that the fully modified microRNA-34a endures for at least 120 hours after being introduced.
“The second hurdle, which entailed fully modifying the microRNA, also significantly reduces the cost of the therapy, but it also is expected to increase patient compliance, improve quality of life, and reduce or eliminate immunogenicity,” Kasinski further explained. “The fully modified microRNA is >400-fold more stable than an unmodified or partially modified version. This increases the duration of the therapy, resulting in less frequent dosing. Fewer doses will be a significant benefit to the patient so they can have more time at home with their families. This will also translate into cost savings as less therapeutic is needed.”
In their reported paper, the team showed that the folate-conjugated FM-miR-34a (FM-FolamiR-34a) could penetrate the dense tissue of tumors and bind to the folate receptor on the cell surface, from where it is then internalized in a vesicle. Once inside the cell, the microRNA-34a escapes the vesicle, and acts to slow cell division. “Using this approach leads to specific delivery to the intended cells at a dose that is 10–100-fold lower than the vehicle used for the failed clinical trial,” Kasinski added. “The ligand (folate)-mediated approach allowed us to significantly reduce dosing, which would help to reduce any potential toxicity (albeit we have yet to identify a toxic dose), and as this moves forward would also reduce cost as less therapeutic is needed.”
There are multiple benefits to using folate-targeting over encapsulation, she further suggested to GEN. “ … folate is a natural substance that is essential in humans … This helps to avoid any potential toxicity that could occur using complex nanoparticles that often have multiple components … with the recent FDA approval of folate-conjugated imaging agents, developed by co-author Dr. Philip Low, that are being used by surgeons to better identify tumor boarders, there is an outstanding body of work that highlights i) safety of folate-conjugates in humans, and ii) rapid and specific delivery of folate-conjugates in human patients.”
The team carried out tests in cultured cells, and in vivo preclinical tests in mice. The results confirmed that the folate-conjugated, fully modified microRNA-34a strongly suppressed the activity of at least three genes—MET, CD44, and AXL—known to drive cancer and resistance to other cancer therapies. “The reported studies confirmed that FM-miR-34a potently inhibited proliferation and invasion, and induced sustained downregulation of endogenous target genes for >120 h following in vivo delivery,” the team noted. “… five days following systemic administration of a single dose of FM-FolamiR-34a, biological targets (MET, CD44, and AXL) were silenced to levels commonly observed following single-gene siRNA targeting.” These results, they suggested, indicate that “the chemical modification does not hinder, but rather enhances, the ability of miR-34a to downregulate its known/predicted targets.”
Experiments evaluating multiple doses of FM-FolamiR-34 confirmed that treatment could slow or reverse tumor growth. Tumors in two treated mice shrank by about 45–75% of their initial volume by the end of the 21-day dosing period, and one animal was completely cured. “Importantly, no significant changes were observed in the body weight throughout the study suggesting the safety of FM-FolamiR-34a,” the investigators noted. Additional tests indicated that the treatment didn’t cause an immune reaction in the recipients. “The full modifications also help to prevent an immune response,” Kasinski commented to GEN. “… the body does not recognize these fully-modified RNAs as foreign, so they are able to enter into the cells and ‘do their job’ without triggering the immune system, a critical issue with the first-generating microRNA therapy that entered into the clinic.”
While further studies will be needed to verify the early results, the overall findings indicate that the team’s approach could be effective on its own and in combination with existing drugs when used against cancers that have built drug resistance. “When we acquired the data, I was ecstatic. I am confident that this approach is better than the current standard of treatment and that there are patients who will benefit from this,” Kasinski noted.
The next stage for the researchers will be to test the treatment in additional model systems and carry out large-scale toxicity studies. “Some models would be used to address efficacy for various other tumors that overexpress the folate receptor, such as lung, colon, and ovarian cancers, adding to our work in breast cancer,” Kasinski noted.
The team expects to focus on TNBC and NSCLC as initial clinical indications, because most of the data so far has been obtained in these two types of tumor, 80% of which overexpress the folate receptor, she added. Ovarian cancer is another possibility, as up to 80% of ovarian cancers also overexpress the folate receptor, although the agent hasn’t yet been tested in this tumor type, Kasinski acknowledged. Nevertheless, “Because the small RNA we are using has been shown to be very effective in tumors lacking p53 signaling, which happens in 50–90% of NSCLC, TNBC, and ovarian cancer we anticipate great results in these cancers.”
It’s also likely that other folate conjugates will also prove to be specific and safe, Kasinski noted. “… the folate conjugates are much smaller than nanoparticles. This affords the therapeutic RNA to penetrate the dense architecture of the tumor microenvironment delivering the RNA deeper into the tumor mass than what can be achieved with nanoparticles.” And due to the simplicity of the folate-delivery system, the synthetic chemistry needed to generate the folate is easier than a complex nanoparticle, she noted. Another major benefit of using folate as a targeting ligand is that it binds very tightly to the folate receptor, which is one of the most overexpressed receptors, “often times representing over one million receptors per cell,” Kasinski explained. “Thus, after a single dose, due to the high affinity and the copy number, over one million copies of miR-34a can get to each of the diseased cells.”
Work will also continue to further improve the miRNA construct. “We have multiple ideas as to how to further improve this agent,” Kasinski noted. “I firmly believe that the agent described in the manuscript meets the stringent criteria that will be needed to gain approval. That being said, in the lab we are working on three additional challenges, that if successful will further improve this agent. These include additional chemistry that could help facility endosomal release of the delivered agent.”
The team is also actively involved in developing ways to increase the circulation half-life of the therapeutic. “While the small size is great for penetrating the tumor tissue, it results in rapid clearance from the body. We have identified a way to maintain the small size and simplistic chemistry while increasing circulation half-life.” Prior to the team’s achievement of stabilizing the RNA, this wasn’t a consideration as the RNA would have just been degraded if it spent more time in circulation, Kasinski pointed out. “The successes we have had with stabilizing the RNA have allowed us to now consider this option. If successful, dosing, and overall cost could be further reduced.” And because the folate-targeting strategy only works for tumors with overexpression of the folate receptor the team is also looking into other small ligands for delivery to other tumors.
“While the idea of using small RNAs as therapeutics is not new, the challenges mentioned above have prevented their advancement,” Kasinski stated. And while the first small RNA, a short-interfering RNA (siRNA) was approved in 2018 for a disease in the liver, she continued, there are no RNA-based therapeutics used for oncology. “It is highly anticipated that our work in oncology will open up the field to a better understanding of what is needed for an effective agent. Particularly for cancer, using this approach one could deliver any small RNA that could ultimately target any gene. It is also not outside of the realm of possibilities to use multiple small RNAs, particularly for treating cancer which is a very heterogenous disease.”